THE STRESS FACTOR
November 27, 2018
 Thanksgiving has come and gone and Christmas is right around the corner – Are you stressed out? This time of year always seems more stressful, but stress in general is hard to avoid. We worry about school, work, finances, illness, children, relationships, and more. Some even worry about how much they worry. Not to add to your stress, but you should be aware that all that worrying could have a negative impact on not only your general health but also your oral health.
Thanksgiving has come and gone and Christmas is right around the corner – Are you stressed out? This time of year always seems more stressful, but stress in general is hard to avoid. We worry about school, work, finances, illness, children, relationships, and more. Some even worry about how much they worry. Not to add to your stress, but you should be aware that all that worrying could have a negative impact on not only your general health but also your oral health.
According to an article in the Journal of Periodontology, there is a strong relationship between stress and periodontal disease (gum disease). In addition to stress, other psychological factors, such as anxiety, depression, and loneliness, are linked to an increased likelihood of periodontal disease.
So how does stressing out about your next car payment, for example, lead to gum disease? Researchers believe that the hormone cortisol may be a factor. Cortisol , also known as the “stress hormone,” is secreted by the adrenal glands and involved in many functions, including proper glucose metabolism, blood pressure regulation, insulin release for blood sugar maintenance, immune function, and inflammatory response. An earlier study published in the same journal the year before found that increased levels of cortisol can lead to more destruction of the gums and bone due to periodontal diseases.
Behavioral factors also may come into play. People who are under extreme amounts of stress or suffering from depression may be more likely to disregard good oral hygiene. They may even take on new behaviors that could negatively impact their oral health, such as the use of nicotine, alcohol, or drugs, all of which can affect the teeth and gums.
Your gums are not the only victims of stress. Another oral side effect is teeth grinding or clenching, which often occurs during sleep. This may lead to headaches, earaches, or toothaches. Facial muscles can become sore and jaw joints tender. Besides causing discomfort, grinding and/or clenching can lead to severe tooth wear, loosening of teeth, and cracked or fractured teeth.
It is important to find healthy things that help relieve stress. A regular exercise routine can do wonders for relieving stress, as well as having a balanced nutritious diet and getting enough sleep. You should be getting 7-8 hours of good sleep every night. If you are not getting that amount, you are depriving yourself of optimal performance.
If you find it difficult to manage your stress, you should see your physician. You should also make your dentist aware of your stress level so that he/she can determine if there are any notable effects going on within your masticatory system and make recommendations to help.
I’ll leave you this week with a quote from A. Cornelius Celsus’s DeMedicina. He was a Roman author and medical historian and wrote this about 2000 years ago.
Live in rooms full of light.
Avoid Heavy food.
Be moderate in the drinking of wine.
Take massage, baths, exercise and gymnastics.
Fight insomnia with gentle rocking or the sound of running water.
Change surroundings and take long journeys.
Strictly avoid frightening ideas.
Indulge in cheerful conversation and amusements.
Listen to music.
Stress cannot be avoided, but it can be managed and minimized by change.
Dr. St. Clair maintains a private dental practice in Rowley and Newburyport dedicated to health-centered family dentistry. If there are certain topics you would like to see written about or questions you have please email them to him at jpstclair@stclairdmd.com. You can view all previously written columns at www.jpeterstclairdentistry.com/blog.
TOXIC FOR DOGS
November 19, 2018
 Xylitol is a sugar substitute that possesses 40 percent fewer calories than sugar and has been shown to help decrease cavities in teeth, among other things. However, it is important to know that xylitol, even in small quantities, is very toxic to dogs.
Xylitol is a sugar substitute that possesses 40 percent fewer calories than sugar and has been shown to help decrease cavities in teeth, among other things. However, it is important to know that xylitol, even in small quantities, is very toxic to dogs.
The dental benefits of xylitol have been known since the 1970’s. Xylitol is not metabolized by the decay-causing bacteria Streptococcus mutans (S. mutans), making it nonacidogenic and thus noncariogenic (not decay causing). Studies have also indicated xylitol decreases the levels of S. mutans in both plaque and saliva. As a result, patients who use xylitol have demonstrated a reduction in decay.
Xylitol is slowly absorbed by the human intestines; as a result, it has minimal side effects on humans. Some may experience minor side effects, mainly stomach upset, although this generally occurs after ingesting large amounts of xylitol (four to five times the recommended amount for cavity prevention). There are studies that the body can adapt to higher dosages of xylitol and that symptoms can subside as the body’s tolerance increases.
While the dental community embraces xylitol for its cavity prevention, many people, including dental professionals, are unaware of its toxic potential – not to humans, but to dogs. While xylitol has little effect on insulin production in humans, dogs can experience a rapid and severe increase in insulin production after just a small amount of xylitol ingestion. A dog that ingests a xylitol equivalent of three to four pieces of gum is at risk for hepatic (liver) failure and necrosis (tissue death).
Dogs tend to be scavengers by nature and their likelihood of encountering potentially toxic substances in and around the house is common. The ASPCA web site lists a multitude of substances, many of which are harmless to humans but potentially dangerous to dogs. Chocolate, grapes, raisins, avocado, onion, and citrus fruits make the list. However, xylitol is unique in that it is contained within foods; as a result, consumers may not even be aware that a product or food item contains xylitol.
For dogs suspected of ingesting xylitol, early intervention is paramount. Prompt medical treatment for uncomplicated xylitol-related hypoglycemia can yield a good prognosis. Once Xylitol has affected the liver, it yields a much graver prognosis.
While veterinarians have been aware of the potential danger of xylitol to dogs for several years, that awareness has escaped most of the dental community – and the general public. This has become a more significant issue as more dental professionals promote products that contain xylitol for its human benefits.
It is important for dog owners to know the different foods and products, such as xylitol, that can be harmful to their pets. Make sure to keep these items out of a dog’s reach – and that includes the garbage. If you suspect ingestion of any of these foods, including xylitol, contact your veterinarian immediately.
Dr. St. Clair maintains a private dental practice in Rowley and Newburyport dedicated to health-centered family dentistry. If there are certain topics you would like to see written about or questions you have please email them to him at jpstclair@stclairdmd.com. You can view all previously written columns at www.jpeterstclairdentistry.com/blog.
Which Holiday Foods Should You Avoid If You Have Sleep Apnea?
 Sleep apnea affects an estimated 22 million people in the U.S. and can have serious consequences to their overall health. In fact, researchers have found a link between sleep apnea and many serious conditions like high blood pressure, depression, weight gain, and stroke. But even if you’re getting treatment for sleep apnea, you might not know that certain foods can aggravate it. With the holiday season upon us, keep reading to learn about which foods you can safely enjoy and which ones you should avoid!
Sleep apnea affects an estimated 22 million people in the U.S. and can have serious consequences to their overall health. In fact, researchers have found a link between sleep apnea and many serious conditions like high blood pressure, depression, weight gain, and stroke. But even if you’re getting treatment for sleep apnea, you might not know that certain foods can aggravate it. With the holiday season upon us, keep reading to learn about which foods you can safely enjoy and which ones you should avoid!
THE SMARTEST OF TEETH
November 13, 2018
Most people who visit the dentist hope they leave the dental office hearing the final salutation from the dentist, “Everything looks great!” Teenagers who have made it without any cavities get used to hearing this…..until the wisdom teeth come into play.
Mother Nature is generous when it comes to our teeth. First, we get 20 baby teeth; next we grow 28 permanent teeth; and finally around age 16-18, we start getting our 4 wisdom teeth (unless of course teeth are congenitally missing).
There are usually 4 wisdom teeth, although some may have as few as none. The removal of wisdom teeth is usually recommended for one of the following reasons:
- When the jaw is not large enough to accommodate the wisdom teeth, causing the teeth to become impacted (unable to grow in) or misaligned.
- When wisdom teeth only partially erupt, leaving an opening for bacteria to enter around the tooth and cause infection.
- When there is a chance that poorly aligned wisdom teeth will damage adjacent teeth.
- When the wisdom teeth, because they are difficult to clean, cause periodontal (gum) problems with adjacent teeth.
- When a cyst (fluid-filled sac) forms and destroys surrounding structures, such as bone or tooth roots.
As soon as it is determined that the wisdom teeth are, or will become partially or fully impacted, they should be removed. This usually occurs between ages 16 to 18, as soon as the jaw has attained the majority of its adult size. Although it is less common, there are times when wisdom teeth will fit and do not need to be removed. You need either a large mouth or small teeth for this to occur.
Removing impacted wisdom teeth at this time has several advantages. First, at this age, the roots are seldom fully formed, even though the tooth has become impacted. If left in place, the tooth will n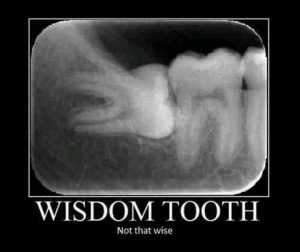 ot erupt any further into the mouth but the roots will continue to grow.
ot erupt any further into the mouth but the roots will continue to grow.
Removing an impacted wisdom tooth before the roots are fully formed is easier and less traumatic for the patient. Also, at this stage in the patient’s development, the bone surrounding the impacted tooth is more pliable. Typically, patients having wisdom teeth removed in their mid-teens heal more rapidly and have a shorter and less complicated postoperative recovery.
There are many adults who still have their wisdom teeth. In my experience, I have seen very few adults who are able to keep their wisdom teeth for their lifetime. They usually cause some kind of problem, which often times does not hurt, as the problem develops. For example, my father-in-law recently needed a partially impacted wisdom tooth removed (which should have been removed about 50 years ago) and lost the molar in front of it because of the damage it had caused.
Today, the vast majority of patients have their wisdom teeth removed in an oral surgeon’s office. It’s not something anyone really wants to do, but the result in most cases is a lifetime of less potential issues. If you still have your wisdom teeth, ask your dentist about their status.
Dr. St. Clair maintains a private dental practice in Rowley and Newburyport dedicated to health-centered family dentistry. If there are certain topics you would like to see written about or questions you have please email them to him at jpstclair@stclairdmd.com. You can view all previously written columns at www.jpeterstclairdentistry.com/blog.
DENTURE MAINTENANCE
November 5, 2018
 Contrary to what many denture-wearers believe, dentures require regular maintenance, including relines, repairs, and replacement. In fact, the average denture should be relined every two to three years and replaced every five to seven years for the most optimal fitting prosthesis. There are many reasons for this maintenance interval and for regular dental examinations, whether or not the patient perceives any problem.
Contrary to what many denture-wearers believe, dentures require regular maintenance, including relines, repairs, and replacement. In fact, the average denture should be relined every two to three years and replaced every five to seven years for the most optimal fitting prosthesis. There are many reasons for this maintenance interval and for regular dental examinations, whether or not the patient perceives any problem.
The first problem has to do with the basic function of the bone surrounding natural teeth. Natural teeth are held in their sockets by thousands of “cables”, called the periodontal ligament that tug and pull on the supporting bone during function. The bone is designed to be strengthened and stimulated in this manner. When the teeth are removed, the bone no longer has appropriate stimulation, and shrinkage occurs unless it is directly loaded again with dental implants. Bone atrophy is accelerated by inappropriate forces caused by loose and ill-fitting dentures.
Relining, or replacing the tissue surface of the denture, helps preserve bone by adapting dentures to the gums as they shrink, but it is only helpful for dentures that are otherwise in good condition, which includes a proper bite relationship. Relining also helps to encourage health of the soft tissues because dentures plastic is porous and becomes heavily laden with bacteria and yeast over time. Relining refreshes the tissue surface of dentures with new acrylic. Sometimes a more advanced type of relining, called rebasing, is the treatment of choice when all of the pink portion of a denture is in poor condition and needs to be replaced.
New dentures should be made when relining or rebasing of dentures can no longer re-establish proper fit and function. Often this is obvious by wear or fracture of the denture teeth. When dentures contribute to headaches or when the patient’s face begins to look “collapsed” or “old”, the need for new dentures is likely.
Lastly, but certainly not of least importance, denture wearers need to stay current with regular dental examinations for inspection of not only the dentures but the tissue for pre-cancerous lesions. Since most people feel they do not need to go to the dentist once they have dentures, many early pre-cancerous lesions are missed.
Everyone is at risk for oral cancer, whether they have teeth or not. In fact, the constant “trauma” and lack of blood circulation caused by chronic denture wear increases the risk for oral cancer development. For this reason alone, annual dental examinations are recommended for denture wearers.
Many patients with older dentures report their dentures fit fine. You can relate this to the fit of shoes. Shoes get broken in over time and seem comfortable. However, the fact is, over time shoes lose their ability to provide proper support. Even though they may be comfortable, they may be causing other problems due to this lack of support.
If you are a denture wearer and have not seen a dentist in a year or more, it’s time to consider a dental visit. Learn about how your dentures are fitting and whether relining or replacing them makes sense. For most, it is also never too late to consider the benefits of dental implants to help preserve bone and secure dentures in place.
Dr. St. Clair maintains a private dental practice in Rowley and Newburyport dedicated to health-centered family dentistry. If there are certain topics you would like to see written about or questions you have please email them to him at jpstclair@stclairdmd.com. You can view all previously written columns at www.jpeterstclairdentistry.com/blog.







